What You Should Know When You Are First Prescribed Oxygen
Editors Note: The experiences shared in this article are those of the author. Please consult your doctor if you feel that you need personalized medical advice.
I have noticed in these forums that doctors and oxygen providers sometimes drop the ball when informing us all of what we need to know when we are first prescribed oxygen.
Needing supplemental oxygen
What is baffling to think about is that I probably needed oxygen about a year before I first started it. The first doctor that I had never checked my oxygen levels until I was in the room and had time to rest after my walk in there.
I questioned him, asking if he thought I needed oxygen, and told him my symptoms of breathlessness after any walking, activity, taking a shower, and dressing for the day. My cousin, who was with me, expressed her concerns as well because she had witnessed these breathing episodes. He just always said that I was fine.
It wasn't until I went to a new doctor after I got insurance that he measured my oxygen, but again I had rested by the time he took it. He did set me up for an overnight sleep study and that was when I was first prescribed oxygen just for sleeping.
The road to getting oxygen prescribed
A month later, I mentioned to my nurse that I was short of breath with activity, so she took it upon herself to give me a six-minute walk test.
In a six-minute walk test, you walk for 6 minutes with a pulsoxometer on. They measure to see how far you can walk and if your oxygen drops as you walk. Any drop below 88 shows that you need oxygen.
At that time, you might get a prescription for oxygen therapy, and your doctor will contact an oxygen supplier who will come titrate (see how much oxygen you need with activity).
Your doctor should send you home information about oxygen. If they don't offer it, be sure to ask.
Also, if you think you are unable to use tanks because of the weight or other problems, you could ask them to write your prescription for a portable oxygen machine rather than tanks. Some oxygen providers will comply, and some will not, but you might need that prescription to get it in most cases.
A learning curve
After the oxygen provider is given your prescription from your doctor, they will come out and get you set up. They will probably titrate you to see how many liters you should be on unless your doctor already did this.
It took a while for me to get used to using oxygen. I think it was my fault that I wasn't told everything that I should know.
I told my doctor and oxygen supplier that I had worked in hospitals and nursing homes and knew how to use oxygen, so I was fine. Little did I know that even though I had worked with oxygen, it differed from using it myself.
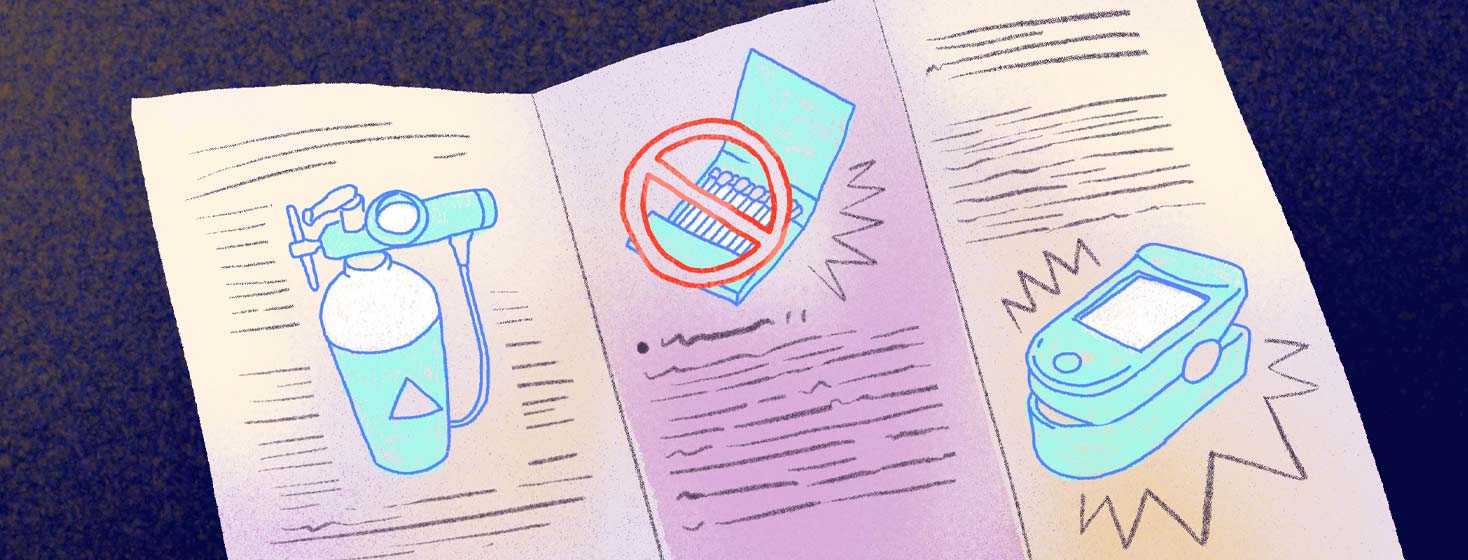
You might get a packet of information on what to do for power outages or any other problems that you may have. Mine brought out a big tank for me to have on hand in case of power outages. Some people will be given a big oxygen machine that can be used 24/7 or with activity.
I was advised never to use more than 50' of hose on your machine. You can take a bath or shower with your oxygen hose on. Just try to keep water out of it.
If you put it up over your shower curtain or through the side of it, it should work just fine. If you do get water in the cannula, be sure to get it dried out well so it doesn't cause an infection.
Be sure to change your nasal cannula once a week and your long hoses once a month. If you are sick or get any holes in your tubing, change them sooner.
Be sure to keep a pulsometer on hand to check your oxygen , and be sure to ask questions. There is no such thing as a dumb question, especially when it comes to our health.
Tips on using oxygen properly
Here are some tips that I have learned along the way. Always ask your oxygen supplier if you have questions.
- Stay 5 feet away from heat sources. That includes gas stoves, candles, lighted fireplaces, and electric or gas heaters.
- Don't use flammable products like cleaning fluid, paint thinner, and aerosol sprays.
- Keep oxygen containers upright. Attach them to a fixed object so they don't topple.
- Skip products with oil, grease, or petroleum. That also goes for petroleum-based creams and ointments like Vaseline on your face or upper chest.
- Have a fire extinguisher close by. Let your fire department know that you have oxygen in your home.
- Tell your electric company if you use an oxygen concentrator so you get priority service in case of a power failure.
Did your doctor or oxygen company explain this all to you, or did you find out on your own? Please share with us in the comments below.
Join the conversation