Your First Exacerbation After Being Diagnosed with COPD - What to Expect
Once you are diagnosed with COPD, emphysema or chronic bronchitis, it is only a matter of time before your first exacerbation strikes. Chances are, it will hit you quite unaware and will be devastating. Some comments I've heard include:
"When I had my first exacerbation, I thought I was going to DIE!"
"Didn't know what hit me and it took 45 minutes to get back into full control."
"That first exacerbation is a big one. We often are unaware and it is a big surprise when it hits. I thought I would die and almost did."
Sound familiar? If not, then you likely are lucky enough to have not had an exacerbation... yet. But rest assured that you will one day, so it's wise to educate yourself. That way, you will be better equipped to take swift action that can help re-stabilize your respiratory status as quickly as possible.
What is a COPD exacerbation?
Exacerbation, pronounced ex-zass-er-bay-shun, is simply a fancy medical term for what lay people generally think of as a severe flare-up or worsening of your COPD symptoms.1 Frequently, it is caused by a respiratory infection. Other times, it may result after inhaling some kind of irritating environmental substance (such as smoke or air pollution). But sometimes there is no real known cause.1
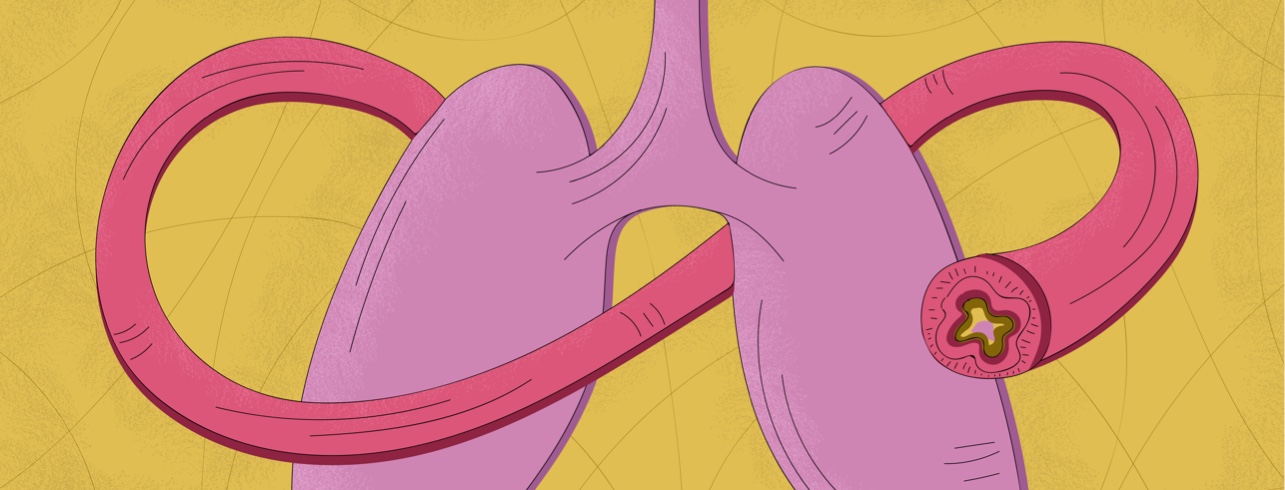
Regardless of the cause, your airways respond by increasing inflammation, which causes:
- Airway tightening
- Swelling in the airways
- Increased mucus in the airways
Those 3 actions combine to increase your everyday COPD symptoms of:1,2
- Coughing more frequently or more intensely
- Breathlessness, even at rest or with routine daily activities
- Changes in the amount, consistency and color of your sputum (also called mucus): clear and thin to thick, yellow, brown or green, perhaps even with specks of blood
- Extra tired (more than usual)
- Problems sleeping or waking up with a headache or feeling confused
- Dipping oxygen levels (if you use a pulse oximeter to monitor)
- Increasing anxiety
These flare-ups sometimes come on gradually over a couple of days, which is why you may not notice what is happening until your symptoms spiral out of control. So, you can see it's important to monitor your respiratory health closely and to be aware of even small changes in your breathing and your symptoms.
What to do if you suspect an exacerbation
Quick action is essential because COPD flare-ups are serious and can even be deadly.1 Getting the right help and treatment early on will make a huge difference in your ultimate health outcome. So, if you even suspect you might be having such a flare-up, don't wait. Call your doctor right away, or if necessary seek out urgent or emergency care.
Do try to stay calm, however. You may already be feeling anxious, and giving in to these feelings can only worsen your symptoms. Rest assured that if you are taking action, then it's a positive step toward relief from how you are feeling in this moment.
How COPD exacerbations are treated
Keep in mind also that COPD flares are treatable. You might feel like you are dying, and if you don't do anything, you could die. But if you get medical help fairly soon after your symptoms worsen, you will recover, in most cases.
One of the first things the doctor will probably do is put you on oxygen.3 Or, if you're already on oxygen, then your liters per minute may be increased temporarily. Or, perhaps they'll switch you from a nasal cannula to a face mask. Other therapies that may be initiated, depending on the cause of your exacerbation, can include:3
- Bronchodilator medicine by inhaler or nebulizer to relax your airways
- Steroid medicine by inhaler, pills or even intravenous to decrease the inflammation
- Antibiotics or antiviral medicines to treat infections
Often, these therapies can be carried out at home. However, if you fail to recover enough despite these interventions, you may need more intensive care. Some patients will benefit from some type of ventilation support.1,3 Noninvasive positive pressure ventilation will often be the first choice, before moving to intubation and a mechanical ventilator. This non-invasive type is sometimes referred to as CPAP or BiPAP.4
Make sure to have a COPD action plan
The best way to deal with the possibility of a severe COPD flare-up is to take a proactive approach. Working with your health care team to develop your own unique COPD Action Plan during your earliest stages of COPD is a smart idea. That way, when your first COPD exacerbation does strike, you'll be ready.
An action plan is nothing more than a step-by-step set of instructions on what actions to take and when should there be changes in your COPD symptoms or respiratory condition. For example, you might be told to:1
- Take your rescue inhaler (a short-acting bronchodilator) every 4 hours
- Fill a standing prescription for a steroid and/or antibiotic
- Call your doctor or seek emergency care
- Increase the flow rate of your supplemental oxygen, if you are already on oxygen, or to use it continuously rather than just at bedtime
Each person's action plan will differ somewhat, depending on his or her current stage of COPD and respiratory condition. Be sure to keep your plan updated as time goes on. And always post it in a visible place within your home and make sure any caregivers are aware of it.
Preventing exacerbations
Flare-ups are an expected part of having COPD. You won't always be able to prevent them from occurring. But there are a few steps you can take that may help decrease their frequency, or even prevent your first one from happening as soon:
- If you are still smoking, make a plan to quit as soon as possible; get help if you need it.
- Do your best to avoid triggers, such as secondhand smoke, car exhaust, chemical fumes and allergic triggers.
- Avoid being around others who are sick, especially those with colds, flu or other respiratory infections.
- Get your yearly flu shot.
Join the conversation